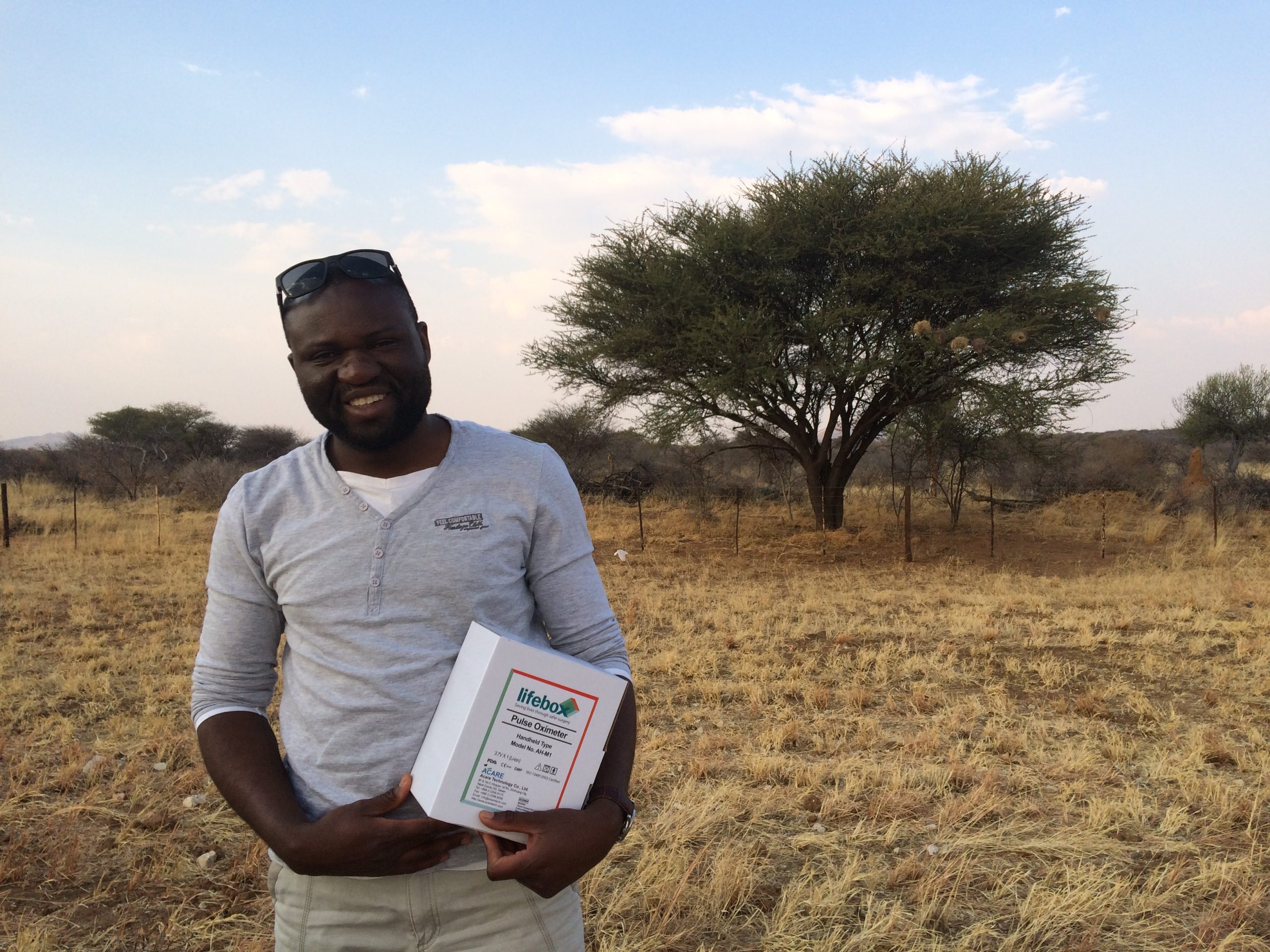
They call him the “Checklist Advocate”
But he’s at home on a mountain bike, powering up one of Namibia’s seven giant hills. He’s at home in the kitchen with his family, while his daughter asks questions about tomato-chopping techniques. And he’s at home in the Operating Room, where he works by turns as both surgeon and anaesthesia provider.
He’s also one of the country’s leading safety experts.
Lifebox met Dr Kabongo in Boston last month (at home in a suit and tie), presenting his methodology and success implementing the Safe Childbirth and Surgical Safety Checklists to our friends at Ariadne Labs. We talked about leadership, safety – and the power of surgery to change lives.

Successful Checklist implementation requires good leadership – it’s not easy, but it’s a fact. Were you always a leader?
I’ve been in a lot of positions of responsibility from a young age. At school I was the head of the class, at university I was the head of our group. It’s just always been like that…
I think leadership is complex, and I like the challenge. It’s the dynamic that makes you think about how to find solutions to complex problems. It’s not just about power – to tell people what to do, have people follow you but it’s the ability to inspire.
I remember the first time my nurse stood and started speaking with some visitors about the Checklist. She spoke with so much passion and inspiration. Everyone said, she’s doing it better than you! I couldn’t have done better. She had embraced the whole thing, and that was amazing. That’s the power of leadership. Here I think I have transformed someone, have inspired someone’s life.

Meanwhile as part of a surgical team there’s a patient on the table and you’re about to have an extraordinary impact on their life. How do you handle that pressure, those decisions?
It can be painful. It’s very emotional at times and you need to find a way to deal with those emotions.
One scenario took place when I was working in rural Zambia, in 2008. I was the only doctor in a community of 36,000 people, 300km from the main town. There was a woman who was experiencing constant bleeding – for long periods of time it wouldn’t stop. She’d had blood transfusions at the main hospital and was sent back to the village. After a while the same issue started up again. She really suffered and was desperate…
I was thinking, what can I do for her? I did a pelvic ultrasound and found she had a huge intra-cavitary fibroid. Usually you’d do a hysterectomy, but she was 26 and she didn’t have a child. She was young, and she wanted one.
I discussed my conclusions with her and told her I had an idea. “I’m going to remove that myoma but not the uterus,” I said. “But if I find myself in trouble I’ll have to remove the womb.” She agreed we could try.
So I took her to the OR, gave her some narcotics, had my nurse monitoring her vitals and used my scalpel on her skin to reach the uterus through a vertical incision. Meticulously I opened it up, dissecting slowly until I reached the cavity. I dissected the whole myoma out, achieved haemostasis and closed. And it was successful! I kept an eye on her, the bleeding stopped, and she went home after one week.
When she came back three months later she’d started having her regular period. She gave me a great gift! She brought me a goat.
How do you take the patient’s wishes into consideration, even when you’re in a life or death situation?
I had another patient who would have lost her fallopian tube after a second concealed ectopic pregnancy, but she said to me “Doctor, I know it’s complicated but please try your best. Give me a chance to have another child.”
So we agreed to do a micro surgery on the tube, and saved her fertility. I’ve never seen someone so happy like that. Perhaps your choice is not always the ‘best’ option, but I think patient involvement, understanding their wishes, is so important. That engagement – that conversation – can even add value to our skills.

The first class of Namibian-trained doctors is graduating this year. What does it mean for the country?
It’s a celebration! It’s great for the country! There is need for more doctors.
How did you become an advocate for the Checklist?
It all started in 2012 at the National Doctors and Dentists Forum where I made a presentation on a STOC (Small Test Of Change) on the Safe Surgery Checklist in our Hospital.
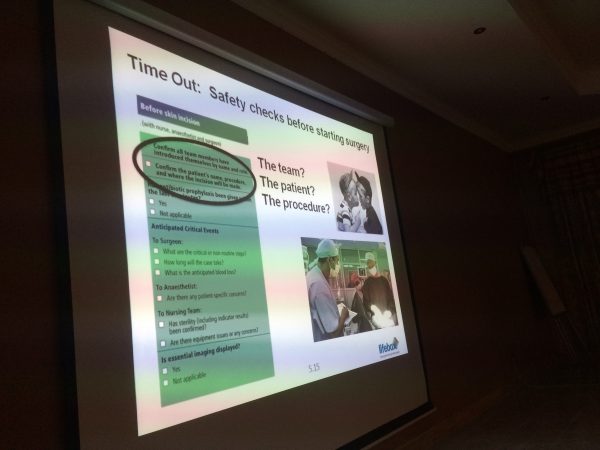
The data was amazing: 25% reduction in perioperative morbidities. This changed the whole picture because it was undisputable local evidence. We had support to continue with the project, so we made it a priority in our district hospital. I was invited at subsequent Quality Improvement meetings to talk about our strategies, since other hospitals were struggling.
The Checklist was already mandated in government hospital OR guidelines, but how many were doing it, or doing it well – that’s a different question.
Checklist use is about translating evidence into practice, but it’s also about culture, the way people do things, and the way we learn from each other. We’ve seen the model really working when people share, communicate and work in a team – approaching adverse events together, and planning changes for the future.
In 2015, I came back to the forum with another Checklist presentation: the Safe Childbirth Checklist. Results were tangible. Guess what happens next? They gave me a nickname. They called me the ‘’Checklist Advocate’’.


