Riddle me this:
What do you call an operation that saves two lives at once?
A caesarean section.
No need to be witty when you’re one of the greatest surgical priorities for healthcare in low-resource settings. An emergency c-section is the most common major procedure in Sub-Saharan Africa: in Rwanda, for example, 2011 saw more than 38,000 urgently undertaken, as opposed to less than 2000 planned.
Safely deliver a struggling baby from a mother, locked in obstructed labour for days and deadly weary, and with one operation you’ve pulled two lives back from certain brink.
But those are the good stories – the truth is, carrying a baby to term and making it to the door of a hospital is still no guarantee of safe delivery. Lack of resources, training and support can make surgery in low-resource settings dangerous, particularly in the rural areas – and that’s before you factor in complex resuscitations, post partum haemorrhage, and conditions far more advanced than would ever be seen in a hospital in a high-resource setting.
In Sub-Saharan Africa, “most deaths are avoidable and one-third are attributable to anaesthesia.” (Dyer, Reed, & James, 2010.)
Simply put, the operation that should save the mother and baby may become the very thing that needlessly ends it.
Today marks another landmark on the road to changing this reality.
In Rwamangana, Rwanda, more than 60 anaesthesia providers have just finished the first day’s sessions – this very minute, in fact (the Lifebox blog has never felt so live!) – of day 1 at the SAFE Obstetrical Anaesthesia course.
Led by faculty from the Rwanda Society of Anesthetists (RSA) and the Canadian Anesthesiologists’ Society International Education Foundation (CAS IEF), the course is supported by the Rwanda Ministry of Health and the World Federation of Societies of Anaesthesiologists (WFSA). It is designed to make a long term impact on the safety and quality of obstetric anaesthesia care.
Over the next few days attendees will develop their skills in obstetric anaesthesia, everything from routine procedures to resuscitation and crisis management.
They’ll flex and strengthen their capacity for teamwork in the operating room through the ‘Building SAFE Teams’ curriculum – confident communication and teamwork being essential for a safe OR, as we well know from the WHO Surgical Safety Checklist.
They’ll get training in how to use Gradian Health Systems’ Universal Anaesthesia Machine (UAM), which is specially designed for use in low-resource settings by a team that knows the importance of safe anaesthesia in safe obstetric care (see Gradian’s recent post on the subject at Every Mother Counts).
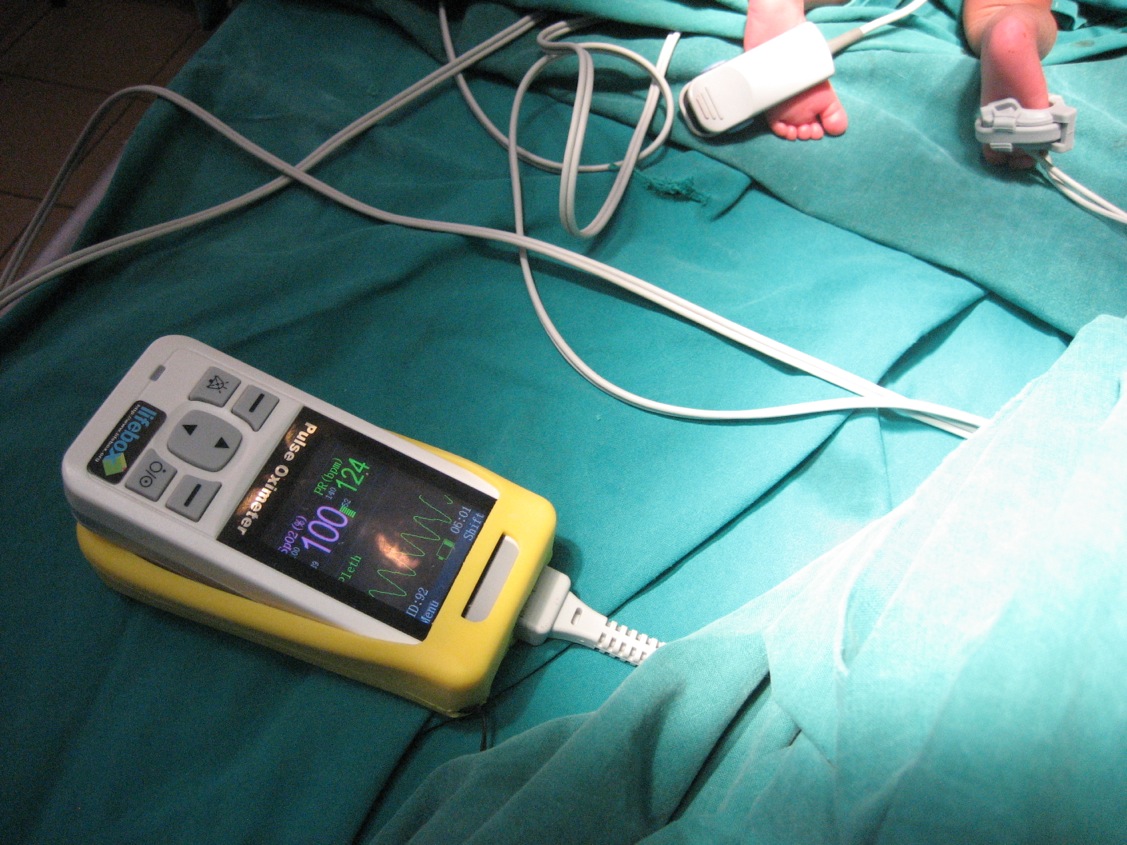
And they’ll leave with Lifebox pulse oximeters – enough, in fact, for every OR in the whole country! Last year CAS led a Make It 0 campaign that succeeded beyond our wildest dreams (combined and totaled). They raised funds for more than 250 oximeters for Rwanda, and we’ll be distributing them at the training course this week.
That’s right – we! Lifebox is thrilled to be joining the team, and over the next few weeks we’ll be sharing photos, tweets (#SAFERwanda), blog posts and more. The course repeats next week with another group of anaesthesia providers – so stand by…