
One Year On as Global CEO of Lifebox:
A dozen countries and hundreds of meetings later, I am more enthusiastic than ever about Lifebox’s work and the global movement in safe surgery and anesthesia that we are part of.
As I reflect on the past year and kick off a regular blog feature for our website, I wanted to highlight five of the lessons I have learned along the way:
Innovate, don’t overcomplicate
 Innovation may be one of the most important and yet overused words in global health and development today. Do not get me wrong, fresh ideas and smart design are essential to improving health services and program delivery.
Innovation may be one of the most important and yet overused words in global health and development today. Do not get me wrong, fresh ideas and smart design are essential to improving health services and program delivery.
But the most effective innovations are not always about finding a new tool or scientific breakthrough: they are using what works in more effective ways.
Take the eponymous Lifebox pulse oximeter. Nobody could argue that monitoring blood oxygen levels during surgery is non-essential and it is why the authors of the WHO Surgical Safety Checklist, and Lifebox’s founders, put the pulse oximeter on the list.
Lifebox did not invent new technology. Instead, they developed an affordable pulse oximeter and adapted to the settings where it is most absent – operating theaters in low-resource countries with over-burdened staff, unreliable electricity, and no means to fix broken equipment.
As one partner said to me recently, the Lifebox pulse oximeter “does what it needs to do and nothing more.”
We need innovation if we are going to meet any of the health needs outlined in the Sustainable Development Goals. I like to think of Lifebox as an “innovative implementer” as we take evidence-based approaches to the tools and techniques that improve surgical safety, and work with our partners to adapt and disseminate them: like the 17,000 oximeters now in the hands of anesthesia providers in over 100 countries.
Checklists Work
 I was already a convert to the power of checklists in global health. Working with Doctors Without Borders/Médecins Sans Frontières (MSF) for fifteen years, I know that following protocols and checklists – and appropriately adapting them to a given context or situation – is crucial for medical teams delivering services in emergencies. Nobody would try to put together massive teams of strangers in a war zone and task them with vaccinating 100,000 kids in a few days, or attempt to treat suspected Ebola cases, without checklists.
I was already a convert to the power of checklists in global health. Working with Doctors Without Borders/Médecins Sans Frontières (MSF) for fifteen years, I know that following protocols and checklists – and appropriately adapting them to a given context or situation – is crucial for medical teams delivering services in emergencies. Nobody would try to put together massive teams of strangers in a war zone and task them with vaccinating 100,000 kids in a few days, or attempt to treat suspected Ebola cases, without checklists.
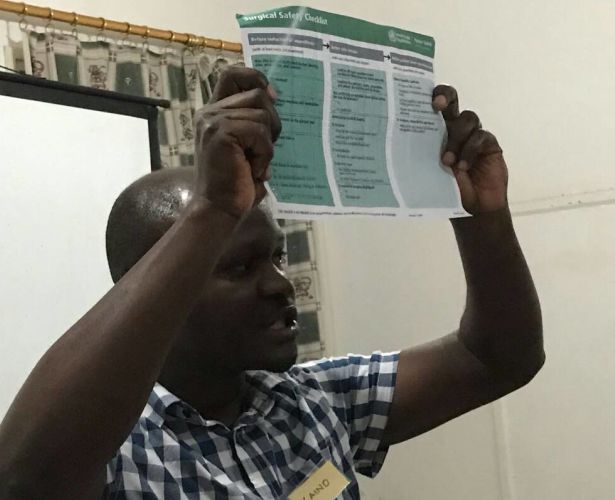
At Lifebox, I have seen the transformative power of checklists in surgery. The WHO Surgical Safety Checklist was created by several Lifebox founders and trustees, including Pauline Philip and Dr. Atul Gawande who wrote a seminal book on its development and impact. Used effectively, it can reduce mortality and complications in surgery by over 40 percent anywhere in the world.
Every surgeon, nurse, anesthesia provider I have spoken with over the past year knows about the WHO Checklist and many use it in their daily work. Of course no piece of paper or laminated wall poster can ensure safety, and there are many obstacles to implementation – teams that don’t communicate, lack of materials from sharp tools to adequate blood supplies. But the beauty of the Checklist is that it helps even the most resource-constrained surgical team focus, step-by-step, on what they need to do to ensure the basic conditions are in place for their patient’s safety.
As Lifebox founder and board member Dr. William Berry said to me when I first took up my post, “Checklist implementation is hard, but we have to chip away at it.” This is true whether in an operating room in South Carolina or South Sudan.
Lifebox’s new Strategic Plan takes the Checklist as an organizing framework. Positive preliminary results from “Clean Cut®”, our checklist-based, team-centered program to reduce surgical infections currently piloting with partners in Ethiopia, show its influence at work. How a piece of paper has helped to spread a culture of safety to operating theaters around the world in just 10 years is nothing less than a ground-shifting global health success story.
Students and Trainees are Forces of Change
 It should be no surprise that I have found students and residents/trainees – ‘the surgical workforce of the future’ – to be the greatest champions of surgical safety, and incredible supporters of Lifebox’s work to create a surgical safety movement. They have grown up with the Checklist, know when it is being used incorrectly, and are not afraid to speak up.
It should be no surprise that I have found students and residents/trainees – ‘the surgical workforce of the future’ – to be the greatest champions of surgical safety, and incredible supporters of Lifebox’s work to create a surgical safety movement. They have grown up with the Checklist, know when it is being used incorrectly, and are not afraid to speak up.
Since 2013, the American Society of Anesthesiologists (ASA) has hosted an annual Resident Lifebox Challenge to encourage anesthesia programs around the US to raise funds for Lifebox. We have been incredibly touched by these Lifebox champions who have organized everything from chili cook-offs to car washes to put pulse oximeters in the hands of their colleagues across the globe. Just as important as the funds they raise is the awareness they are building about global surgery needs.
The students of InciSioN, the global surgical student society, have allowed Lifebox to reach audiences we never otherwise would. Their global volunteer network translated The Checklist Effect – Lifebox’s documentary about surgical safety filmed and directed by Lauren Anders Brown and produced by Lifebox’s Sarah Kessler – into 11 languages (and growing!). I am amazed by their enthusiasm, energy, and drive to facilitate change.
Professional Societies are Drivers of Progress
 I have spent the past year learning a whole new set of acronyms for the many professional societies operating at national, regional, and international levels that Lifebox partners with. The World Federation of the Societies of Anaesthesiologists (WFSA) and the Association of Anaesthetists of Great Britain and Ireland (AAGBI) are Lifebox founding partners and remain our closest allies in working to improve surgical safety (as well as our hosts and office-mates in London!). Our partners in Australia, New Zealand and the United States are also essential supporters and champions.
I have spent the past year learning a whole new set of acronyms for the many professional societies operating at national, regional, and international levels that Lifebox partners with. The World Federation of the Societies of Anaesthesiologists (WFSA) and the Association of Anaesthetists of Great Britain and Ireland (AAGBI) are Lifebox founding partners and remain our closest allies in working to improve surgical safety (as well as our hosts and office-mates in London!). Our partners in Australia, New Zealand and the United States are also essential supporters and champions.
Throughout the past year I have been impressed by the work of surgical, nursing, pediatric, and anesthesia professional societies in improving access to safe surgery globally. My first year as CEO was book-ended by attending the West African College of Surgeons (WACS) meeting in Burkina Faso in February and, in December, the annual meeting of the College of Surgeons of East, Southern, and Central Africa (COSECSA) with a dose of Latin American anesthesiology in the middle at the Confederation of Latin American Societies of Anesthesia (CLASA) meeting in Uruguay.
I have been warned that there are some societies that can be reluctant to change practices, even when evidence suggests otherwise. But I truly believe that Lifebox’s success is largely due to our practical partnerships with professional societies. They are vital for promoting surgical safety, encouraging research and data collection on needs and best practices, building the surgical workforce, and demanding resources for safe surgery in their countries, regions, and internationally.
Just today in Ethiopia, I attended a new course called “SAFE OR” taught by a combined Ethiopian and international group of surgeons, nurses, and anesthesiologists to 32 Ethiopian surgical team members. Never before have these groups taught or been taught together. By working across professional societies and partnering together to address the core of surgical safety – teamwork – SAFE OR is an excellent example of how professional associations can work together to promote lasting improvements in surgical safety.
Global Surgery Needs to Demand Resources
 When I speak with groups about Lifebox, I have taken up a line of questioning Dr. Gawande often uses: How many of you have had surgery? How many of you have a family member who has had surgery?
When I speak with groups about Lifebox, I have taken up a line of questioning Dr. Gawande often uses: How many of you have had surgery? How many of you have a family member who has had surgery?
Usually about 90 percent of the people in the room – depending on age group! – raise their hands.
The fact that 5 billion people do not have access to adequate surgical services is worth repeating again and again. I constantly find myself checking this number and the lack of commensurate attention or funding of surgical services, locally and internationally. It seems so unbelievably huge.
Unfortunately, if you have worked on access to medicines for HIV, TB or malaria, you know that simply stating dramatic statistics does not move resources or action. Building a movement does.
Countries are doing what they have been asked to: developing national surgical, anesthesia, and obstetric plans, often with great support from outside partners like Harvard’s PGSSC. But now that they have the plans, how will they be funded? Programming can be as cost-effective as possible but improving the safety of surgery and increasing access will cost money. There is no way around it. We need to work on data, costing, and plans to make use of limited resources to improve surgery – but we also need to work together to identify and fight for funding sources for global surgery and anesthesia.
After a year of meeting dozens of inspiring global surgical and anaesthesia champions, I truly believe we are on the cusp of a powerful global surgery movement. I have been inspired by resolutions passed at the World Health Assembly on surgery as an essential part of Universal Health Coverage, by advocacy groups like the G4 Alliance and funders such as the GE Foundation who are working across professional siloes to devote increased resources to ensure all patients the right to safe and affordable surgery.
I feel lucky to be a part of this movement and look forward to everything we will accomplish in the coming years.

