The Antibiotic Timeout: Tackling Antibiotic Overuse in Surgery
Developing an Antibiotic Stewardship Program to support safer surgical care in low-resource settings
Antibiotics used during surgery comprise a major part of antibiotic use worldwide: One in every six inpatient antibiotic prescriptions are for preventing infections in surgical patients.
Antibiotic resistance, where bacteria evolve to be protected from the effects of the antibiotic that is meant to kill them, causes the death of millions of people every year. The use – and misuse and overuse – of antibiotics is a driving force behind this growing global health issue.
Sub-Saharan Africa is believed to have the highest burden of antimicrobial resistance worldwide, with staggeringly high levels of resistance found in commonly used antibiotics.
Data from the global implementation of Lifebox’s surgical infection reduction program – Clean Cut – has illuminated the extent of antibiotic over-prescribing: With more than 90% of patients receiving antibiotics after surgery. The prescription of antibiotics after surgery to prevent infections is against the World Health Organization (WHO) recommendations and does not reduce rates of surgical infection.
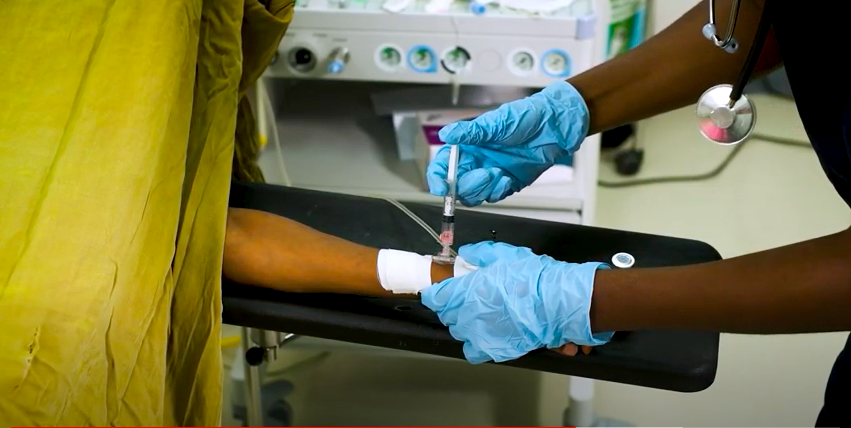
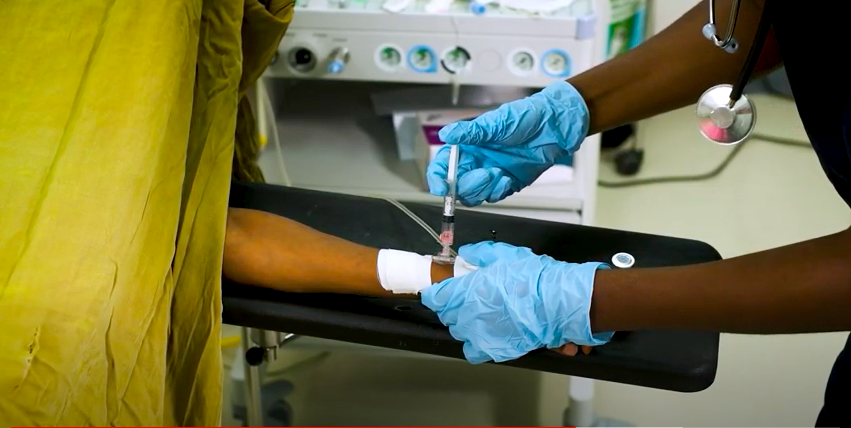
Administering antibiotics in the operating room, prior to surgery, to reduce risk of surgical infection
The proper administration of antibiotics is one of the key standards of the Lifebox surgical infection reduction program – Clean Cut. To be effective, antibiotics must be administered to the surgical patient within 60 minutes before incision to reduce the risk of infection.
However in many low-resource settings, where sterility practices are variable and the rates of surgical infection are high, the routine prescribing of antibiotics after surgery is commonly taught. International guidelines also do not account for differences in resource-constrained environments where recommended antibiotics may not be available and national guidelines often fail to contextualize recommendations – resulting in poor adherence to the guidelines.
As well as not reducing rates of infection, the subscription of antibiotics after surgery contributes to the overuse of antibiotics and extends the length of hospital stay for patients.
This is where Lifebox steps in.
Surgical infections are a major barrier to reducing antibiotic prescriptions, with high infection rates driving high antibiotic use. Although antibiotics after surgery have not been shown to prevent infections, alternative infection prevention processes are challenging in resource-limited settings. The Clean Cut program reduces rates of surgical infection by strengthening six key infection prevention standards – providing better infection prevention tools and resulting in fewer antibiotics needing to be prescribed.
To build on this work, Lifebox is developing ‘The Antibiotic Timeout’ – an antibiotic stewardship program. The program is developing a contextualized antibiotic protocol to apply national and international guidelines to the local setting. The protocol will be piloted at five partner hospitals in Ethiopia and Rwanda in the coming months – with 2,250 surgical patients participating.
This work is supported by the NIH Fogarty International Center Global Health Equity Scholars Program (NIH FIC TW010540) and a seed grant from the Stanford Center for Innovation in Global Health, funded by the Stanford Department of Surgery.

