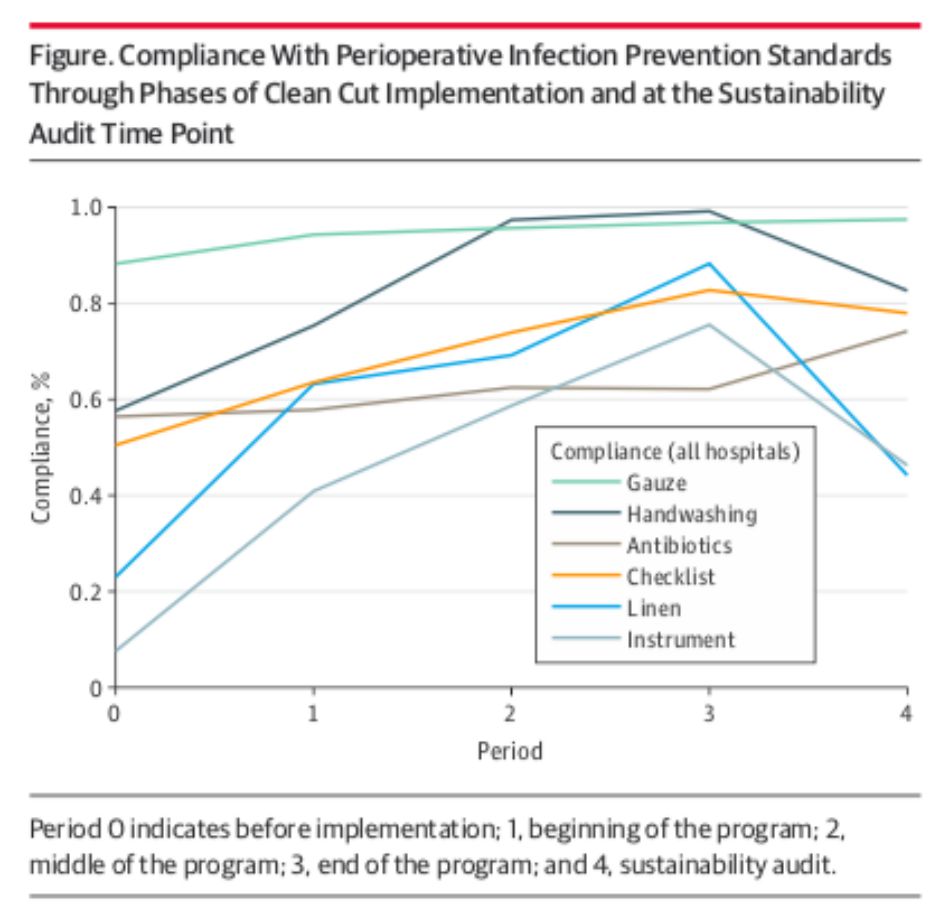
Surgical site infections (SSIs) are the leading hospital acquired infection in low- and middle-income countries – where rates of infection are more than double that found in the United States1. Clean Cut, a quality improvement intervention developed by the global non-profit Lifebox, supports surgical teams in addressing the causes of SSIs by improving adherence to six infection prevention practices, including the appropriate timing of antibiotics and confirmation of instrument sterility. The sustainability audit also shows compliance continued to improve across four of the practices compared with the post-implementation period: surgical safety checklist use (58.4% vs 50.0%), skin antisepsis (74.8% vs 57.6%), antibiotic prophylaxis (65.7% vs 58.7%), and gauze counting (94.7% vs 93.9%).Some attrition in compliance occurred with surgical linen integrity and sterility (46.0% vs 39.0%) and instrument sterility (54.7% vs 41.8%), but performance in these two areas remained above baseline (6.2% and 7.7%, respectively).

Sustainable Results for Tackling Surgical Infection
New Research Shows Lasting Impact of Lifebox Clean Cut Program - published in The Journal of the American Medical Association (JAMA) Surgery.
The results of the lasting impact of Lifebox’s surgical infection reduction program – Clean Cut – have been published in The Journal of the American Medical Association (JAMA) Surgery.
“Sustainability of a Surgical Quality Improvement Program at Hospitals in Ethiopia” details the results of a follow up audit conducted at seven hospitals in a cohort of 3,385 surgical patients six to eighteen months after completion of the program. The results demonstrate that compared to baseline, hospitals maintained improvements in compliance with all six program infection prevention standards, indicating the lasting behavior changes achieved by Clean Cut.
“These positive results demonstrate the ability of Clean Cut to achieve lasting improvements in the safety of surgical patients. This study is further evidence that interventions to increase surgical quality and infection prevention behaviors are essential investments for long-term improvements in patient safety.”Dr. Nichole Starr, general surgery resident at UCSF and lead author.
New Research Shows Lasting Impact of Lifebox Clean Cut Program - published in The Journal of the American Medical Association (JAMA) Surgery.
“These welcome results show the lasting impact of Lifebox’s work in Ethiopia without the need for major resource investment. In partnership with the Federal Ministry of Health of Ethiopia, Clean Cut has impacted more than 80,000 surgical patients to date and we are excited to replicate this success in other locations.”
Dr. Natnael Gebeyehu Admasu, general surgery resident at Tikur Anbessa Hospital, Addis Ababa and Lifebox Fellow
A previous study – published in the British Journal of Surgery in September 2020 – showed Clean Cut resulted in a 35% reduction in the risk of SSIs in all surgical patients. Lifebox is scaling the Clean Cut program across Ethiopia in partnership with the Federal Ministry of Health, impacting more than 80,000 surgical patients to date, and is replicating the program in Liberia and Madagascar.
- GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infectious Diseases. 2018;18(5):516-525.2 Forrester JA, Starr N, Negussie T, Schaps D, Adem M, Alemu S,et al.Clean Cut (adaptive, multimodal surgical infection prevention programme) for low-resource settings: a prospective quality improvement study. Br J Surg. Published online September 21, 2020. https://bjssjournals.onlinelibrary.wiley.com/doi/full/10.1002/bjs.11997
“These welcome results show the lasting impact of Lifebox’s work in Ethiopia without the need for major resource investment. In partnership with the Federal Ministry of Health of Ethiopia, Clean Cut has impacted more than 80,000 surgical patients to date and we are excited to replicate this success in other locations.”Dr. Natnael Gebeyehu Admasu, general surgery resident at Tikur Anbessa Hospital, Addis Ababa and Lifebox Fellow
A previous study – published in the British Journal of Surgery in September 2020 – showed Clean Cut resulted in a 35% reduction in the risk of SSIs in all surgical patients. Lifebox is scaling the Clean Cut program across Ethiopia in partnership with the Federal Ministry of Health, impacting more than 80,000 surgical patients to date, and is replicating the program in Liberia and Madagascar.
- GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infectious Diseases. 2018;18(5):516-525.2 Forrester JA, Starr N, Negussie T, Schaps D, Adem M, Alemu S,et al.Clean Cut (adaptive, multimodal surgical infection prevention programme) for low-resource settings: a prospective quality improvement study. Br J Surg. Published online September 21, 2020. https://bjssjournals.onlinelibrary.wiley.com/doi/full/10.1002/bjs.11997

